- Review
- Open access
- Published:
Sexual and reproductive health implementation research in humanitarian contexts: a scoping review
Reproductive Health volume 21, Article number: 64 (2024)
Abstract
Background
Meeting the health needs of crisis-affected populations is a growing challenge, with 339 million people globally in need of humanitarian assistance in 2023. Given one in four people living in humanitarian contexts are women and girls of reproductive age, sexual and reproductive health care is considered as essential health service and minimum standard for humanitarian response. Despite growing calls for increased investment in implementation research in humanitarian settings, guidance on appropriate methods and analytical frameworks is limited.
Methods
A scoping review was conducted to examine the extent to which implementation research frameworks have been used to evaluate sexual and reproductive health interventions in humanitarian settings. Peer-reviewed papers published from 2013 to 2022 were identified through relevant systematic reviews and a literature search of Pubmed, Embase, PsycInfo, CINAHL and Global Health databases. Papers that presented primary quantitative or qualitative data pertaining to a sexual and reproductive health intervention in a humanitarian setting were included.
Results
Seven thousand thirty-six unique records were screened for inclusion, and 69 papers met inclusion criteria. Of these, six papers explicitly described the use of an implementation research framework, three citing use of the Consolidated Framework for Implementation Research. Three additional papers referenced other types of frameworks used in their evaluation. Factors cited across all included studies as helping the intervention in their presence or hindering in their absence were synthesized into the following Consolidated Framework for Implementation Research domains: Characteristics of Systems, Outer Setting, Inner Setting, Characteristics of Individuals, Intervention Characteristics, and Process.
Conclusion
This review found a wide range of methodologies and only six of 69 studies using an implementation research framework, highlighting an opportunity for standardization to better inform the evidence for and delivery of sexual and reproductive health interventions in humanitarian settings. Increased use of implementation research frameworks such as a modified Consolidated Framework for Implementation Research could work toward both expanding the evidence base and increasing standardization.
Plain English summary
Three hundred thirty-nine million people globally were in need of humanitarian assistance in 2023, and meeting the health needs of crisis-affected populations is a growing challenge. One in four people living in humanitarian contexts are women and girls of reproductive age, and provision of sexual and reproductive health care is considered to be essential within a humanitarian response. Implementation research can help to better understand how real-world contexts affect health improvement efforts. Despite growing calls for increased investment in implementation research in humanitarian settings, guidance on how best to do so is limited. This scoping review was conducted to examine the extent to which implementation research frameworks have been used to evaluate sexual and reproductive health interventions in humanitarian settings. Of 69 papers that met inclusion criteria for the review, six of them explicitly described the use of an implementation research framework. Three used the Consolidated Framework for Implementation Research, a theory-based framework that can guide implementation research. Three additional papers referenced other types of frameworks used in their evaluation. This review summarizes how factors relevant to different aspects of implementation within the included papers could have been organized using the Consolidated Framework for Implementation Research. The findings from this review highlight an opportunity for standardization to better inform the evidence for and delivery of sexual and reproductive health interventions in humanitarian settings. Increased use of implementation research frameworks such as a modified Consolidated Framework for Implementation Research could work toward both expanding the evidence base and increasing standardization.
Background
Over the past few decades, the field of public health implementation research (IR) has grown as a means by which the real-world conditions affecting health improvement efforts can be better understood. Peters et al. put forward the following broad definition of IR for health: “IR is the scientific inquiry into questions concerning implementation – the act of carrying an intention into effect, which in health research can be policies, programmes, or individual practices (collectively called interventions)” [1].
As IR emphasizes real-world circumstances, the context within which a health intervention is delivered is a core consideration. However, much IR implemented to date has focused on higher-resource settings, with many proposed frameworks developed with particular utility for a higher-income setting [2]. In recognition of IR’s potential to increase evidence across a range of settings, there have been numerous reviews of the use of IR in lower-resource settings as well as calls for broader use [3, 4]. There have also been more focused efforts to modify various approaches and frameworks to strengthen the relevance of IR to low- and middle-income country settings (LMICs), such as the work by Means et al. to adapt a specific IR framework for increased utility in LMICs [2].
Within LMIC settings, the centrality of context to a health intervention’s impact is of particular relevance in humanitarian settings, which present a set of distinct implementation challenges [5]. Humanitarian responses to crisis situations operate with limited resources, under potential security concerns, and often under pressure to relieve acute suffering and need [6]. Given these factors, successful implementation of a particular health intervention may require different qualities than those that optimize intervention impact under more stable circumstances [7]. Despite increasing recognition of the need for expanded evidence of health interventions in humanitarian settings, the evidence base remains limited [8]. Furthermore, despite its potential utility, there is not standardized guidance on IR in humanitarian settings, nor are there widely endorsed recommendations for the frameworks best suited to analyze implementation in these settings.
Sexual and reproductive health (SRH) is a core aspect of the health sector response in humanitarian settings [9]. Yet, progress in addressing SRH needs has lagged far behind other services because of challenges related to culture and ideology, financing constraints, lack of data and competing priorities [10]. The Minimum Initial Service Package (MISP) for SRH in Crisis Situations is the international standard for the minimum set of SRH services that should be implemented in all crisis situations [11]. However, as in other areas of health, there is need for expanded evidence for planning and implementation of SRH interventions in humanitarian settings. Recent systematic reviews of SRH in humanitarian settings have focused on the effectiveness of interventions and service delivery strategies, as well as factors affecting utilization, but have not detailed whether IR frameworks were used [12,13,14,15]. There have also been recent reviews examining IR frameworks used in various settings and research areas, but none have explicitly focused on humanitarian settings [2, 16].
Given the need for an expanded evidence base for SRH interventions in humanitarian settings and the potential for IR to be used to expand the available evidence, a scoping review was undertaken. This scoping review sought to identify IR approaches that have been used in the last ten years to evaluate SRH interventions in humanitarian settings.
This review also sought to shed light on whether there is a need for a common framework to guide research design, analysis, and reporting for SRH interventions in humanitarian settings and if so, if there are any established frameworks already in use that would be fit-for-purpose or could be tailored to meet this need.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews was utilized to guide the elements of this review [17]. The review protocol was retrospectively registered with the Open Science Framework (https://osf.io/b5qtz).
Search strategy
A two-fold search strategy was undertaken for this review, which covered the last 10 years (2013–2022). First, recent systematic reviews pertaining to research or evaluation of SRH interventions in humanitarian settings were identified through keyword searches on PubMed and Google Scholar. Four relevant systematic reviews were identified [12,13,14,15] Table 1.
Second, a literature search mirroring these reviews was conducted to identify relevant papers published since the completion of searches for the most recent review (April 2017). Additional file 1 includes the search terms that were used in the literature search [see Additional file 1].
The literature search was conducted for papers published from April 2017 to December 2022 in the databases that were searched in one or more of the systematic reviews: PubMed, Embase, PsycInfo, CINAHL and Global Health. Searches were completed in January 2023 Table 2.
Screening
Two reviewers screened each identified study for alignment with inclusion criteria. Studies in the four systematic reviews identified were considered potentially eligible if published during the last 10 years. These papers then underwent full-text review to confirm satisfaction of all inclusion criteria, as inclusion criteria were similar but not fully aligned across the four reviews.
Literature search results were exported into a citation manager (Covidence), duplicates were removed, and a step-wise screening process for inclusion was applied. First, all papers underwent title and abstract screening. The remaining papers after abstract screening then underwent full-text review to confirm satisfaction of all inclusion criteria. Title and abstract screening as well as full-text review was conducted independently by both authors; disagreements after full-text review were resolved by consensus.
Data extraction and synthesis
The following content areas were summarized in Microsoft Excel for each paper that met inclusion criteria: publication details including author, year, country, setting [rural, urban, camp, settlement], population [refugees, internally displaced persons, general crisis-affected], crisis type [armed conflict, natural disaster], crisis stage [acute, chronic], study design, research methods, SRH intervention, and intervention target population [specific beneficiaries of the intervention within the broader population]; the use of an IR framework; details regarding the IR framework, how it was used, and any rationale given for the framework used; factors cited as impacting SRH interventions, either positively or negatively; and other key findings deemed relevant to this review.
As the focus of this review was on the approach taken for SRH intervention research and evaluation, the quality of the studies themselves was not assessed.
Results
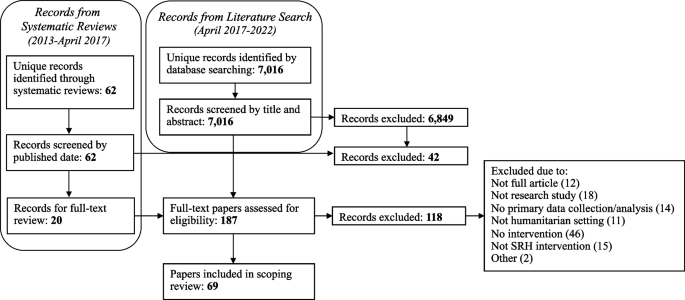
Twenty papers underwent full-text review due to their inclusion in one or more of the four systematic reviews and meeting publication date inclusion criteria. The literature search identified 7,016 unique papers. After full-text screening, 69 met all inclusion criteria and were included in the review. Figure 1 illustrates the search strategy and screening process.
Papers published in each of the 10 years of the review timeframe (2013–2022) were included. 29% of the papers originated from the first five years of the time frame considered for this review, with the remaining 71% papers coming from the second half. Characteristics of included publications, including geographic location, type of humanitarian crisis, and type of SRH intervention, are presented in Table 3.
A wide range of study designs and methods were used across the papers, with both qualitative and quantitative studies well represented. Twenty-six papers were quantitative evaluations [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43], 17 were qualitative [44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60], and 26 used mixed methods [61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86]. Within the quantitative evaluations, 15 were observational, while five were quasi-experimental, five were randomized controlled trials, and one was an economic evaluation. Study designs as classified by the authors of this review are summarized in Table 4.
Six papers (9%) explicitly cited use of an IR framework. Three of these papers utilized the Consolidated Framework for Implementation Research (CFIR) [51, 65, 70]. The CFIR is a commonly used determinant framework that—in its originally proposed form in 2009—is comprised of five domains, each of which has constructs to further categorize factors that impact implementation. The CFIR domains were identified as core content areas influencing the effectiveness of implementation, and the constructs within each domain are intended to provide a range of options for researchers to select from to “guide diagnostic assessments of implementation context, evaluate implementation progress, and help explain findings.” [87] To allow for consistent terminology throughout this review, the original 2009 CFIR domains and constructs are used.
Guan et al. conducted a mixed methods study to assess the feasibility and effectiveness of a neonatal hepatitis B immunization program in a conflict-affected rural region of Myanmar. Guan et al. report mapping data onto the CFIR as a secondary analysis step. They describe that “CFIR was used as a comprehensive meta-theoretical framework to examine the implementation of the Hepatitis B Virus vaccination program,” and implementation themes from multiple study data sources (interviews, observations, examination of monitoring materials) were mapped onto CFIR constructs. They report their results in two phases – Pre-implementation training and community education, and Implementation – with both anchored in themes that they had mapped onto CFIR domains and constructs. All but six constructs were included in their analysis, with a majority summarized in a table and key themes explored further in the narrative text. They specify that most concerns were identified within the Outer Setting and Process domains, while elements identified within the Inner Setting domain provided strength to the intervention and helped mitigate against barriers [70].
Sarker et al. conducted a qualitative study to assess provision of maternal, newborn and child health services to Rohingya refugees residing in camps in Cox’s Bazar, Bangladesh. They cite using CFIR as a guide for thematic analysis, applying it after a process of inductive and deductive coding to index these codes into the CFIR domains. They utilized three of the five CFIR domains (Outer Setting, Inner Setting, and Process), stating that the remaining two domains (Intervention Characteristics and Characteristics of Individuals) were not relevant to their analysis. They then proposed two additional CFIR domains, Context and Security, for use in humanitarian contexts. In contrast to Guan et al., CFIR constructs are not used nor mentioned by Sarker et al., with content under each domain instead synthesized as challenges and potential solutions. Regarding the CFIR, Sarker et al. write, “The CFIR guided us for interpretative coding and creating the challenges and possible solutions into groups for further clarification of the issues related to program delivery in a humanitarian crisis setting.” [51]
Sami et al. conducted a mixed methods case study to assess the implementation of a package of neonatal interventions at health facilities within refugee and internally displaced persons camps in South Sudan. They reference use of the CFIR earlier in the study than Sarker et al., basing their guides for semi-structured focus group discussions on the CFIR framework. They similarly reference a general use of the CFIR framework as they conducted thematic analysis. Constructs are referenced once, but they do not specify whether their application of the CFIR framework included use of domains, constructs, or both. This may be in part because they then applied an additional framework, the World Health Organization (WHO) Health System Framework, to present their findings. They describe a nested approach to their use of these frameworks: “Exploring these [CFIR] constructs within the WHO Health Systems Framework can identify specific entry points to improve the implementation of newborn interventions at critical health system building blocks.” [65]
Three papers cite use of different IR frameworks. Bolan et al. utilized the Theoretical Domains Framework in their mixed methods feasibility study and pilot cluster randomized trial evaluating pilot use of the Safe Delivery App by maternal and newborn health workers providing basic emergency obstetric and newborn care in facilities in the conflict-affected Maniema province of the Democratic Republic of the Congo (DRC). They used the Theroetical Domains Framework in designing interview questions, and further used it as the coding framework for their analysis. Similar to the CFIR, the Theoretical Domains Framework is a determinant framework that consists of domains, each of which then includes constructs. Bolan et al. utilized the Theoretical Domains Framework at the construct level in interview question development and at the domain level in their analysis, mapping interview responses to eight of the 14 domains [83]. Berg et al. report using an “exploratory design guided by the principles of an evaluation framework” developed by the Medical Research Council to analyze the implementation process, mechanisms of impact, and outcomes of a three-pillar training intervention to improve maternal and neonatal healthcare in the conflict-affected South Kivu province of the DRC [67, 88]. Select components of this evaluation framework were used to guide deductive analysis of focus group discussions and in-depth interviews [67]. In their study of health workers’ knowledge and attitudes toward newborn health interventions in South Sudan, before and after training and supply provision, Sami et al. report use of the Conceptual Framework of the Role of Attitudes in Evidence-Based Practice Implementation in their analysis process. The framework was used to group codes following initial inductive coding analysis of in-depth interviews [72].
Three other papers cite use of specific frameworks in their intervention evaluation [19, 44, 76]. As a characteristic of IR is the use of an explicit framework to guide the research, the use of the frameworks in these three papers meets the intention of IR and serves the purpose that an IR framework would have in strengthening the analytical rigor. Castle et al. cite use of their program’s theory of change as a framework for a mixed methods evaluation of the provision of family planning services and more specifically uptake of long-acting reversible contraception use in the DRC. They describe use of the theory of change to “enhance effectiveness of [long-acting reversible contraception] access and uptake.” [76] Thommesen et al. cite use of the AAAQ (Availability, Accessibility, Acceptability and Quality) framework in their qualitative study assessing midwifery services provided to pregnant women in Afghanistan. This framework is focused on the “underlying elements needed for attainment of optimum standard of health care,” but the authors used it in this paper to evaluate facilitators and barriers to women accessing midwifery services [44]. Jarrett et al. cite use of the Centers for Disease Control and Prevention’s (CDC) Guidelines for Evaluating Public Health Surveillance Systems to explore the characteristics of a population mobility, mortality and birth surveillance system in South Kivu, DRC. Use of these CDC guidelines is cited as one of four study objectives, and commentary is included in the Results section pertaining to each criteria within these guidelines, although more detail regarding use of these guidelines or the authors’ experience with their use in the study is not provided [19].
Overall, 22 of the 69 papers either explicitly or implicitly identified IR as relevant to their work. Nineteen papers include a focus on feasibility (seven of which did not otherwise identify the importance of exploring questions concerning implementation), touching on a common outcome of interest in implementation research [89].
While a majority of papers did not explicitly or implicitly use an IR framework to evaluate their SRH intervention of focus, most identified factors that facilitated implementation when they were present or served as a barrier when absent. Sixty cite factors that served as facilitators and 49 cite factors that served as barriers, with just three not citing either. Fifty-nine distinct factors were identified across the papers.
Three of the six studies that explicitly used an IR framework used the CFIR, and the CFIR is the only IR framework that was used by multiple studies. As previously mentioned, Means et al. put forth an adaptation of the CFIR to increase its relevance in LMIC settings, proposing a sixth domain (Characteristics of Systems) and 11 additional constructs [2]. Using the expanded domains and constructs as proposed by Means et al., the 59 factors cited by papers in this review were thematically grouped into the six domains: Characteristics of Systems, Outer Setting, Inner Setting, Characteristics of Individuals, Intervention Characteristics, and Process. Within each domain, alignment with CFIR constructs was assessed for, and alignment was found with 29 constructs: eight of Means et al.’s 11 constructs, and 21 of the 39 standard CFIR constructs. Three factors did not align with any construct (all fitting within the Outer Setting domain), and 14 aligned with a construct label but not the associated definition. Table 5 synthesizes the mapping of factors affecting SRH intervention implementation to CFIR domains and constructs, with the construct appearing in italics if it is considered to align with that factor by label but not by definition.
Table 6 lists the CFIR constructs that were not found to have alignment with any factor cited by the papers in this review.
Discussion
This scoping review sought to assess how IR frameworks have been used to bolster the evidence base for SRH interventions in humanitarian settings, and it revealed that IR frameworks, or an explicit IR approach, are rarely used. All four of the systematic reviews identified with a focus on SRH in humanitarian settings articulate the need for more research examining the effectiveness of SRH interventions in humanitarian settings, with two specifically citing a need for implementation research/science [12, 13]. The distribution of papers across the timeframe included in this review does suggest that more research on SRH interventions for crisis-affected populations is taking place, as a majority of relevant papers were published in the second half of the review period. The papers included a wide range of methodologies, which reflect the differing research questions and contexts being evaluated. However, it also invites the question of whether there should be more standardization of outcomes measured or frameworks used to guide analysis and to facilitate increased comparison, synthesis and application across settings.
Three of the six papers that used an IR framework utilized the CFIR. Guan et al. used the CFIR at both a domain and construct level, Sarker et al. used the CFIR at the domain level, and Sami et al. did not specify which CFIR elements were used in informing the focus group discussion guide [51, 65, 70]. It is challenging to draw strong conclusions about the applicability of CFIR in humanitarian settings based on the minimal use of CFIR and IR frameworks within the papers reviewed, although Guan et al. provides a helpful model for how analysis can be structured around CFIR domains and constructs. It is worth considering that the minimal use of IR frameworks, and more specifically CFIR constructs, could be in part because that level of prescriptive categorization does not allow for enough fluidity in humanitarian settings. It also raises questions about the appropriate degree of standardization to pursue for research done in these settings.
The mapping of factors affecting SRH intervention implementation provides an example of how a modified CFIR framework could be used for IR in humanitarian contexts. This mapping exercise found factors that mapped to all five of the original CFIR domains as well as the sixth domain proposed by Means et al. All factors fit well within the definition for the selected domain, indicating an appropriate degree of fit between these existing domains and the factors identified as impacting SRH interventions in humanitarian settings. On a construct level, however, the findings were more variable, with one-quarter of factors not fully aligning with any construct. Furthermore, over 40% of the CFIR constructs (including the additional constructs from Means et al.) were not found to align with any factors cited by the papers in this review, also demonstrating some disconnect between the parameters posed by the CFIR constructs and the factors cited as relevant in a humanitarian context.
It is worth noting that while the CFIR as proposed in 2009 was used in this assessment, as well as in the included papers which used the CFIR, an update was published in 2022. Following a review of CFIR use since its publication, the authors provide updates to construct names and definitions to “make the framework more applicable across a range of innovations and settings.” New constructs and subconstructs were also added, for a total of 48 constructs and 19 subconstructs across the five domains [90]. A CFIR Outcomes Addendum was also published in 2022, based on recommendations for the CFIR to add outcomes and intended to be used as a complement to the CFIR determinants framework [91]. These expansions to the CFIR framework may improve applicability of the CFIR in humanitarian settings. Several constructs added to the Outer Setting domain could be of particular utility – critical incidents, local attitudes, and local conditions, each of which could help account for unique challenges faced in contexts of crisis. Sub-constructs added within the Inner Setting domain that seek to clarify structural characteristics and available resources would also be of high utility based on mapping of the factors identified in this review to the original CFIR constructs. As outcomes were not formally included in the CFIR until the 2022 addendum, a separate assessment of implementation outcomes was not undertaken in this review. However, analysis of the factors cited by papers in this review as affecting implementation was derived from the full text of the papers and thus captures content relevant to implementation determinants that is contained within the outcomes.
Given the demonstrated need for additional flexibility within an IR framework for humanitarian contexts, while not a focus of this review, it is worth considering whether a different framework could provide a better fit than the CFIR. Other frameworks have differing points of emphasis that would create different opportunities for flexibility but that do not seem to resolve the challenges experienced in applying the CFIR to a humanitarian context. As one example, the EPIS (Exploration, Preparation, Implementation, Sustainment) Framework considers the impact of inner and outer context on each of four implementation phases; while the constructs within this framework are broader than the CFIR, an emphasis on the intervention characteristics is missing, a domain where stronger alignment within the CFIR is also needed [92]. Alternatively, the PRISM (Practical, Robust Implementation and Sustainability Model) framework is a determinant and evaluation framework that adds consideration of context factors to the RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) outcomes framework. It has a stronger emphasis on intervention aspects, with sub-domains to account for both organization and patient perspectives within the intervention. While PRISM does include aspects of context, external environment considerations are less robust and intentionally less comprehensive in scope, which would not provide the degree of alignment possible between the Characteristics of Systems and Outer Setting CFIR domains for the considerations unique to humanitarian environments [93].
Reflecting on their experience with the CFIR, Sarker et al. indicate that it can be a “great asset” in both evaluating current work and developing future interventions. They also encourage future research of humanitarian health interventions to utilize the CFIR [51]. The other papers that used the CFIR do not specifically reflect on their experience utilizing it, referring more generally to having felt that it was a useful tool [65, 70]. On their use of an evaluation framework, Berg et al. reflected that it lent useful structure and helped to identify aspects affecting implementation that otherwise would have gone un-noticed [67]. The remaining studies that utilized an IR framework did not specifically comment on their experience with its use [72, 83]. While a formal IR framework was not engaged by other studies, a number cite a desire for IR to contribute further detail to their findings [21, 37].
In their recommendations for strengthening the evidence base for humanitarian health interventions, Ager et al. speak to the need for “methodologic innovation” to develop methodologies with particular applicability in humanitarian settings [7]. As IR is not yet routinized for SRH interventions, this could be opportune timing for the use of a standardized IR framework to gauge its utility. Using an IR framework to assess factors influencing implementation of the MISP in initial stages of a humanitarian response, and interventions to support more comprehensive SRH service delivery in protracted crises, could lend further rigor and standardization to SRH evaluations, as well as inform strategies to improve MISP implementation over time. Based on categorizing factors identified by these papers as relevant for intervention evaluation, there does seem to be utility to a modified CFIR approach. Given the paucity of formal IR framework use within SRH literature, it would be worth conducting similar scoping exercises to assess for explicit use of IR frameworks within the evidence base for other health service delivery areas in humanitarian settings. In the interim, the recommended approach from this review for future IR on humanitarian health interventions would be a modified CFIR approach with domain-level standardization and flexibility for constructs that may standardize over time with more use. This would enable use of a common analytical framework and vocabulary at the domain level for stakeholders to describe interventions and the factors influencing the effectiveness of implementation, with constructs available to use and customize as most appropriate for specific contexts and interventions.
This review had a number of limitations. As this was a scoping review and a two-part search strategy was used, the papers summarized here may not be comprehensive of those written pertaining to SRH interventions over the past 10 years. Papers from 2013 to 2017 that would have met this scoping review’s inclusion criteria may have been omitted due to being excluded from the systematic reviews. The review was limited to papers available in English. Furthermore, this review did not assess the quality of the papers included or seek to assess the methodology used beyond examination of the use of an IR framework. It does, however, serve as a first step in assessing the extent to which calls for implementation research have been addressed, and identify entry points for strengthening the science and practice of SRH research in humanitarian settings.
With one in 23 people worldwide in need of humanitarian assistance, and financing required for response plans at an all-time high, the need for evidence to guide resource allocation and programming for SRH in humanitarian settings is as important as ever [94]. Recent research agenda setting initiatives and strategies to advance health in humanitarian settings call for increased investment in implementation research—with priorities ranging from research on effective strategies for expanding access to a full range of contraceptive options to integrating mental health and psychosocial support into SRH programming to capturing accurate and actionable data on maternal and perinatal mortality in a wide range of acute and protracted emergency contexts [95, 96]. To truly advance guidance in these areas, implementation research will need to be conducted across diverse humanitarian settings, with clear and consistent documentation of both intervention characteristics and outcomes, as well as contextual and programmatic factors affecting implementation.
Conclusions
Implementation research has potential to increase impact of health interventions particularly in crisis-affected settings where flexibility, adaptability and context-responsive approaches are highlighted as cornerstones of effective programming. There remains significant opportunity for standardization of research in the humanitarian space, with one such opportunity occurring through increased utilization of IR frameworks such as a modified CFIR approach. Investing in more robust sexual and reproductive health research in humanitarian contexts can enrich insights available to guide programming and increase transferability of learning across settings.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AAAQ:
-
Availability, Accessibility, Acceptability and Quality
- CDC:
-
Centers for Disease Control and Prevention
- CFIR:
-
Consolidated Framework for Implementation Research
- DRC:
-
Democratic Republic of the Congo
- EPIS:
-
Exploration, Preparation, Implementation, Sustainment
- IR:
-
Implementation research
- LMIC:
-
Low and middle income country
- MISP:
-
Minimum Initial Service Package
- PRISM:
-
Practical, Robust Implementation and Sustainability Model
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RE-AIM:
-
Reach, Effectiveness, Adoption, Implementation, Maintenance
- SRH:
-
Sexual and reproductive health
- WHO:
-
World Health Organization
References
Peters DH, et al. Implementation research: what it is and how to do it. RESEARCH METHODS. 2013;347:7.
Means AR, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci. 2020;15(1):17.
Alonge O, et al. How is implementation research applied to advance health in low-income and middle-income countries? BMJ Glob Health. 2019;4(2):e001257.
Ridde V, Pérez D, Robert E. Using implementation science theories and frameworks in global health. BMJ Glob Health. 2020;5(4):e002269.
Gaffey MF, et al. Delivering health and nutrition interventions for women and children in different conflict contexts: a framework for decision making on what, when, and how. Lancet (London, England). 2021;397(10273):543–54.
Singh NS, et al. Delivering health interventions to women, children, and adolescents in conflict settings: what have we learned from ten country case studies? The Lancet. 2021;397(10273):533–42.
Ager A, et al. Strengthening the evidence base for health programming in humanitarian crises. Science. 2014;345(6202):1290–2.
Blanchet K, et al. Evidence on public health interventions in humanitarian crises. The Lancet. 2017;390(10109):2287–96.
Sphere A. The Sphere Handbook | Standards for quality humanitarian response. 2018.
Barot S. In a State of Crisis: Meeting the Sexual and Reproductive Health Needs of Women in Humanitarian Situations. Guttmacher Policy Rev. 2017;20:7.
Crisis, I.-A.W.G.f.R.H.i., Minimum Initial Service Package. 2020: https://www.unfpa.org/resources/minimum-initial-service-package-misp-srh-crisis-situations.
Casey SE. Evaluations of reproductive health programs in humanitarian settings: a systematic review. Confl Heal. 2015;9(1):S1.
Singh NS, et al. A long way to go: a systematic review to assess the utilisation of sexual and reproductive health services during humanitarian crises. BMJ Glob Health. 2018;3(2):e000682.
Singh NS, et al. Evaluating the effectiveness of sexual and reproductive health services during humanitarian crises: A systematic review. PLoS ONE. 2018;13(7):e0199300.
Warren E, et al. Systematic review of the evidence on the effectiveness of sexual and reproductive health interventions in humanitarian crises. BMJ Open. 2015;5(12):e008226.
Dadich A, Piper A, Coates D. Implementation science in maternity care: a scoping review. Implement Sci. 2021;16(1):16.
Tricco AC, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Devine A, et al. Strategies for the prevention of perinatal hepatitis B transmission in a marginalized population on the Thailand-Myanmar border: a cost-effectiveness analysis. BMC Infect Dis. 2017;17(1):552.
Jarrett P, et al. Evaluation of a population mobility, mortality, and birth surveillance system in South Kivu. Democratic Republic of the Congo Disasters. 2020;44(2):390–407.
Logie CH, et al. A Psycho-Educational HIV/STI Prevention Intervention for Internally Displaced Women in Leogane, Haiti: Results from a Non-Randomized Cohort Pilot Study. PLoS ONE. 2014;9(2):e89836.
O’Laughlin KN, et al. A cohort study to assess a communication intervention to improve linkage to HIV care in Nakivale Refugee Settlement. Uganda Glob Public Health. 2021;16(12):1848–55.
Adam I. The influence of maternal health education on the place of delivery in conflict settings of Darfur. Sudan Conflict and Health. 2015;9:31.
Adam IF, et al. Relationship between implementing interpersonal communication and mass education campaigns in emergency settings and use of reproductive healthcare services: evidence from Darfur, Sudan. BMJ Open. 2015;5(9):e008285.
Edmond K, et al. Mobile outreach health services for mothers and children in conflict-affected and remote areas: a population-based study from Afghanistan. Arch Dis Child. 2020;105(1):18–25.
Nasir S, et al. Dissemination and implementation of the e-MCHHandbook, UNRWA’s newly released maternal and child health mobile application: a cross-sectional study. BMJ Open. 2020;10(3):e034885.
O’Laughlin KN, et al. Feasibility and acceptability of home-based HIV testing among refugees: a pilot study in Nakivale refugee settlement in southwestern Uganda. BMC Infect Dis. 2018;18(1):332.
Adam I. Evidence from cluster surveys on the association between home-based counseling and use of family planning in conflict-affected Darfur. Int J Gynecol Obstet. 2016;133(2):221–5.
Casey S, et al. Availability of long-acting and permanent family-planning methods leads to increase in use in conflict-affected northern Uganda: Evidence from cross-sectional baseline and endline cluster surveys. Glob Public Health. 2013;8(3):284–97.
Corna F, et al. Supporting maternal mental health of Rohingya refugee women during the perinatal period to promote child health and wellbeing: a field study in Cox’s Bazar. Intervention, the Journal of Mental Health & Psychosocial Support in Conflict Affected Areas. 2019;17(2):160–8.
Glass N, et al. Effectiveness of the Communities Care programme on change in social norms associated with gender-based violence (GBV) with residents in intervention compared with control districts in Mogadishu, Somalia. BMJ Open. 2019;9(3):e023819.
James LE, et al. Development and Testing of a Community-Based Intervention to Address Intimate Partner Violence among Rohingya and Syrian Refugees: A Social Norms-Based Mental Health-Integrated Approach. Int J Environ Res Public Health. 2021;18(21):11674.
Le Roux E, et al. Engaging with faith groups to prevent VAWG in conflict-affected communities: results from two community surveys in the DRC. BMC Int Health Hum Rights. 2020;20(1):27.
Morris CN, et al. When political solutions for acute conflict in Yemen seem distant, demand for reproductive health services is immediate: a programme model for resilient family planning and post-abortion care services. Sex Reprod Health Matters. 2019;27(2):1610279.
Anibueze AU, et al. Impact of counseling visual multimedia on use of family planning methods among displaced Nigerian families. Health Promot Int. 2022;37(3):daac060.
Doocy S, et al. Cash-based assistance and the nutrition status of pregnant and lactating women in the Somalia food crisis: A comparison of two transfer modalities. PLoS ONE. 2020;15(4):e0230989.
Draiko CV, et al. The effect of umbilical cord cleansing with chlorhexidine gel on neonatal mortality among the community births in South Sudan: a quasi-experimental study. Pan Afr Med J. 2021;38:78.
Edmond KM, et al. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Med. 2018;16(1):106.
Edmond KM, et al. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries, a prospective population based intervention study from Afghanistan. BMC Pregnancy Childbirth. 2019;19(1):193.
Bakesiima R, et al. Effect of peer counselling on acceptance of modern contraceptives among female refugee adolescents in northern Uganda: A randomised controlled trial. PLoS ONE. 2021;16(9):e0256479.
Greene MC, et al. Evaluation of an integrated intervention to reduce psychological distress and intimate partner violence in refugees: Results from the Nguvu cluster randomized feasibility trial. PLoS ONE. 2021;16(6):e0252982.
Gupta J, et al. Gender norms and economic empowerment intervention to reduce intimate partner violence against women in rural Côte d’Ivoire: a randomized controlled pilot study. BMC Int Health Hum Rights. 2013;13(1):46.
Hossain M, et al. Working with men to prevent intimate partner violence in a conflict-affected setting: a pilot cluster randomized controlled trial in rural Côte d’Ivoire. BMC Public Health. 2014;14(1):339.
Vaillant J, et al. Engaging men to transform inequitable gender attitudes and prevent intimate partner violence: a cluster randomised controlled trial in North and South Kivu, Democratic Republic of Congo. BMJ Glob Health. 2020;5(5):e002223.
Thommesen T, et al. “The midwife helped me … otherwise I could have died”: women’s experience of professional midwifery services in rural Afghanistan - a qualitative study in the provinces Kunar and Laghman. BMC Pregnancy Childbirth. 2020;20(1):140.
Awasom-Fru A, et al. Doctors’ experiences providing sexual and reproductive health care at Catholic Hospitals in the conflict-affected North-West region of Cameroon: a qualitative study. Reprod Health. 2022;19(1):126.
Kabakian-Khasholian T, Makhoul J, Ghusayni A. “A person who does not have money does not enter”: a qualitative study on refugee women’s experiences of respectful maternity care. BMC Pregnancy and Childbirth. 2022;22(1):748.
Lilleston P, et al. Evaluation of a mobile approach to gender-based violence service delivery among Syrian refugees in Lebanon. Health Policy Plan. 2018;33(7):767–76.
Mugo NS, et al. Barriers Faced by the Health Workers to Deliver Maternal Care Services and Their Perceptions of the Factors Preventing Their Clients from Receiving the Services: A Qualitative Study in South Sudan. Matern Child Health J. 2018;22(11):1598–606.
Persson M, et al. A qualitative study on health care providers’ experiences of providing comprehensive abortion care in Cox’s Bazar, Bangladesh. Conflict and Health. 2021;15(1):6.
Phanwichatkul T, et al. The perceptions and practices of Thai health professionals providing maternity care for migrant Burmese women: An ethnographic study. Women Birth. 2022;35(4):e356–68.
Sarker M, et al. Effective maternal, newborn and child health programming among Rohingya refugees in Cox’s Bazar, Bangladesh: Implementation challenges and potential solutions. PLoS ONE. 2020;15(3):e0230732.
Tousaw E, et al. “Without this program, women can lose their lives”: migrant women’s experiences with the Safe Abortion Referral Programme in Chiang Mai. Thailand Reprod Health Matters. 2017;25(51):58–68.
Tousaw E, et al. “It is just like having a period with back pain”: exploring women’s experiences with community-based distribution of misoprostol for early abortion on the Thailand-Burma border. Contraception. 2018;97(2):122–9.
West L, et al. Factors in use of family planning services by Syrian women in a refugee camp in Jordan. Journal of Family Planning and Reproductive Health Care. 2017;43(2):96–102.
O’Connell KA, et al. Meeting the Sexual and Reproductive Health Needs of Internally Displaced Persons in Ethiopia’s Somali Region: A Qualitative Process Evaluation. Glob Health Sci Pract. 2022;10(5):e2100818.
Orya E, et al. Strengthening close to community provision of maternal health services in fragile settings: an exploration of the changing roles of TBAs in Sierra Leone and Somaliland. BMC Health Serv Res. 2017;17(1):460.
Perera SM, et al. Barriers to seeking post-abortion care in Paktika Province, Afghanistan: a qualitative study of clients and community members. BMC Womens Health. 2021;21(1):390.
Tanabe M, et al. Piloting community-based medical care for survivors of sexual assault in conflict-affected Karen State of eastern Burma. Confl Heal. 2013;7(1):12.
Tran NT, et al. Clinical outreach refresher trainings in crisis settings (S-CORT): clinical management of sexual violence survivors and manual vacuum aspiration in Burkina Faso, Nepal, and South Sudan. Reprod Health Matters. 2017;25(51):103–13.
Yankah E, et al. Feasibility and acceptability of mobile phone platforms to deliver interventions to address gender-based violence among Syrian adolescent girls and young women in Izmir. Turkey Vulnerable Children and Youth Studies. 2020;15(2):133–43.
Muuo S, et al. Barriers and facilitators to care-seeking among survivors of gender-based violence in the Dadaab refugee complex. Sex Reprod Health Matters. 2020;28(1):1722404.
Amsalu R, et al. Essential newborn care practice at four primary health facilities in conflict affected areas of Bossaso, Somalia: a cross-sectional study. Conflict and Health. 2019;13(13):27.
Myers A, et al. Facilitators and barriers in implementing the Minimum Initial Services Package (MISP) for reproductive health in Nepal post-earthquake. Conflict and Health. 2018;12:35.
Santo L.C.d, et al. Feasibility and acceptability of a video library tool to support community health worker counseling in rural Afghan districts: a cross-sectional assessment. Conflict and Health. 2020;14:56.
Sami S, et al. Understanding health systems to improve community and facility level newborn care among displaced populations in South Sudan: a mixed methods case study. BMC Pregnancy Childbirth. 2018;18(1):325.
Amsalu R, et al. Effectiveness of clinical training on improving essential newborn care practices in Bossaso, Somalia: a pre and postintervention study. BMC Pediatr. 2020;20(1):215.
Berg M, Mwambali SN, Bogren M. Implementation of a three-pillar training intervention to improve maternal and neonatal healthcare in the Democratic Republic Of Congo: a process evaluation study in an urban health zone. Glob Health Action. 2022;15(1):2019391.
Castillo M, et al. Turning Disaster into an Opportunity for Quality Improvement in Essential Intrapartum and Newborn Care Services in the Philippines: Pre- to Posttraining Assessments. Biomed Res Int. 2016;2016:1–9.
Foster AM, Arnott G, Hobstetter M. Community-based distribution of misoprostol for early abortion: evaluation of a program along the Thailand-Burma border. Contraception. 2017;96(4):242–7.
Guan TH, et al. Implementation of a neonatal hepatitis B immunization program in rural Karenni State, Myanmar: A mixed-methods study. PLoS ONE. 2021;16(12):e0261470.
Logie, C.H., et al., Mixed-methods findings from the Ngutulu Kagwero (agents of change) participatory comic pilot study on post-rape clinical care and sexual violence prevention with refugee youth in a humanitarian setting in Uganda. Global Public Health, 2022((Logie C.H., carmen.logie@utoronto.ca) Factor-Inwentash Faculty of Social Work, University of Toronto, Toronto, Canada(Logie C.H., carmen.logie@utoronto.ca) Women’s College Research Institute, Women’s College Hospital, Toronto, Canada(Logie C.H., carmen.l).
Sami S, et al. “You have to take action”: changing knowledge and attitudes towards newborn care practices during crisis in South Sudan. Reprod Health Matters. 2017;25(51):124–39.
Smith JR, et al. Clinical care for sexual assault survivors multimedia training: a mixed-methods study of effect on healthcare providers’ attitudes, knowledge, confidence, and practice in humanitarian settings. Confl Heal. 2013;7(1):14.
Stevens A, et al. Folate supplementation to prevent birth abnormalities: evaluating a community-based participatory action plan for refugees and migrant workers on the Thailand-Myanmar border. Public Health. 2018;161:83–9.
Nguyen Toan T, et al. Strengthening healthcare providers’ capacity for safe abortion and postabortion care services in humanitarian settings: lessons learned from the clinical outreach refresher training model (S-CORT) in Uganda, Nigeria, and the Democratic Republic of Congo. Conflict and Health. 2021;15(1):20.
Castle S, et al. Successful programmatic approaches to facilitating IUD uptake: CARE’s experience in DRC. BMC Womens Health. 2019;19(1):104.
Deitch J, et al. “They Love Their Patients”: Client Perceptions of Quality of Postabortion Care in North and South Kivu, the Democratic Republic of the Congo. Global health, science and practice. 2019;7(Suppl 2):S285–98.
Ferreyra C, et al. Evaluation of a community-based HIV test and start program in a conflict affected rural area of Yambio County, South Sudan. PLoS ONE. 2021;16(7):e0254331.
Ho LS, Wheeler E. Using Program Data to Improve Access to Family Planning and Enhance the Method Mix in Conflict-Affected Areas of the Democratic Republic of the Congo. Glob Health Sci Pract. 2018;6(1):161–77.
Klabbers RE, et al. Health Worker Perspectives on Barriers and Facilitators of Assisted Partner Notification for HIV for Refugees and Ugandan Nationals: A Mixed Methods Study in West Nile Uganda. AIDS Behav. 2021;25(10):3206–22.
Turner C, et al. Neonatal Intensive Care in a Karen Refugee Camp: A 4 Year Descriptive Study. PLoS ONE. 2013;8(8):e72721.
Vries Id, et al. Key lessons from a mixed-method evaluation of a postnatal home visit programme in the humanitarian setting of Gaza. Eastern Mediterr Health J. 2021;27(6):546–52.
Bolan NE, et al. mLearning in the Democratic Republic of the Congo: A Mixed-Methods Feasibility and Pilot Cluster Randomized Trial Using the Safe Delivery App. Global health, science and practice. 2018;6(4):693–710.
Khan MN, et al. Evaluating feasibility and acceptability of a local psycho-educational intervention for pregnant women with common mental problems affected by armed conflict in Swat, Pakistan: A parallel randomized controlled feasibility trial. Int J Soc Psychiatry. 2017;63(8):724–35.
Hynes M, et al. Using a quality improvement approach to improve maternal and neonatal care in North Kivu, Democratic Republic of Congo. Reprod Health Matters. 2017;25(51):140–50.
Gibbs A, et al. The impacts of combined social and economic empowerment training on intimate partner violence, depression, gender norms and livelihoods among women: an individually randomised controlled trial and qualitative study in Afghanistan. BMJ Glob Health. 2020;5(3):e001946.
Damschroder L, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science: IS; 2009.
Moore GF, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258.
Proctor E, et al. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm Policy Ment Health. 2011;38(2):65–76.
Damschroder LJ, et al. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Damschroder LJ, et al. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR Outcomes Addendum. Implement Sci. 2022;17(1):7.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a Conceptual Model of Evidence-Based Practice Implementation in Public Service Sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38(1):4–23.
Feldstein AC, Glasgow RE. A Practical, Robust Implementation and Sustainability Model (PRISM) for Integrating Research Findings into Practice. The Joint Commission Journal on Quality and Patient Safety. 2008;34(4):228–43.
OCHA. Global Humanitarian Overview 2023. 2022 [cited 2023 8/3/2023]; Available from: https://humanitarianaction.info/node/13073/article/glance-0. Accessed 8 Mar 2023.
Kobeissi L, et al. Setting research priorities for sexual, reproductive, maternal, newborn, child and adolescent health in humanitarian settings. Confl Heal. 2021;15(1):16.
Save the, C., et al. Roadmap to Accelerate Progress for Every Newborn in Humanitarian Settings 2020 – 2024. 2020. p. 52.
Inter-Agency Working Group on Reproductive Health in, C. Inter-Agency Field Manual on Reproductive Health in Humanitarian Settings. 2018.
Acknowledgements
Not applicable.
Funding
The authors received no funding for this study.
Author information
Authors and Affiliations
Contributions
AN and HT designed the scoping review. AN conducted the literature search. AN and HT screened records for inclusion. AN extracted data from included studies. Both authors contributed to synthesis of results. AN drafted the manuscript and both authors contributed to editorial changes.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Literature search terms: Exact search terms used in literature search, with additional detail on the methodology to determine search terms and definitions used for each component of the search
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Norton, A., Tappis, H. Sexual and reproductive health implementation research in humanitarian contexts: a scoping review. Reprod Health 21, 64 (2024). https://doi.org/10.1186/s12978-024-01793-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01793-2